Our Senses & Arousal: The Power of Smell
Let's talk about the power of smell and the important role it plays in building arousal and heightening intimacy.
Feminists-Against-Faking-It
If you're having orgasm-less sex, it's time to speak up and take action. Here are our tips to help communicate with your partner and empower yourself to stop faking it!
Tips To Help Alleviate Menopause Symptoms
In honor of Menopause Awareness Month, Maureen shares 12 tips to help alleviate menopause symptoms.
Pleasure After Trauma
For trauma survivors, physical intimacy can trigger feelings of shame, fear, anxiety, and even discomfort. Certified Sex Therapist and Clinical Sexologist Holly Wood gives advice on how trauma survivors can reclaim pleasure and learn to feel safe and connected again.
Finding Samantha's Lost Orgasm | Bathtub Masturbation On Sex And The City
Samantha of Sex and the City taught us it was okay to enjoy sex and pursue pleasure without shame. In a classic episode, Samantha struggles to have an orgasm and turns to bathtub masturbation to get the job done.

Porn Star Dani Daniels Dispels Bathtub Masturbation Myth
Porn star, sex toy expert, and self-proclaimed water masturbator Dani Daniels raves how the WaterSlyde makes fauceting comfortable and dispels the myth that the water pressure from a bathtub faucet isn't strong enough to get you off.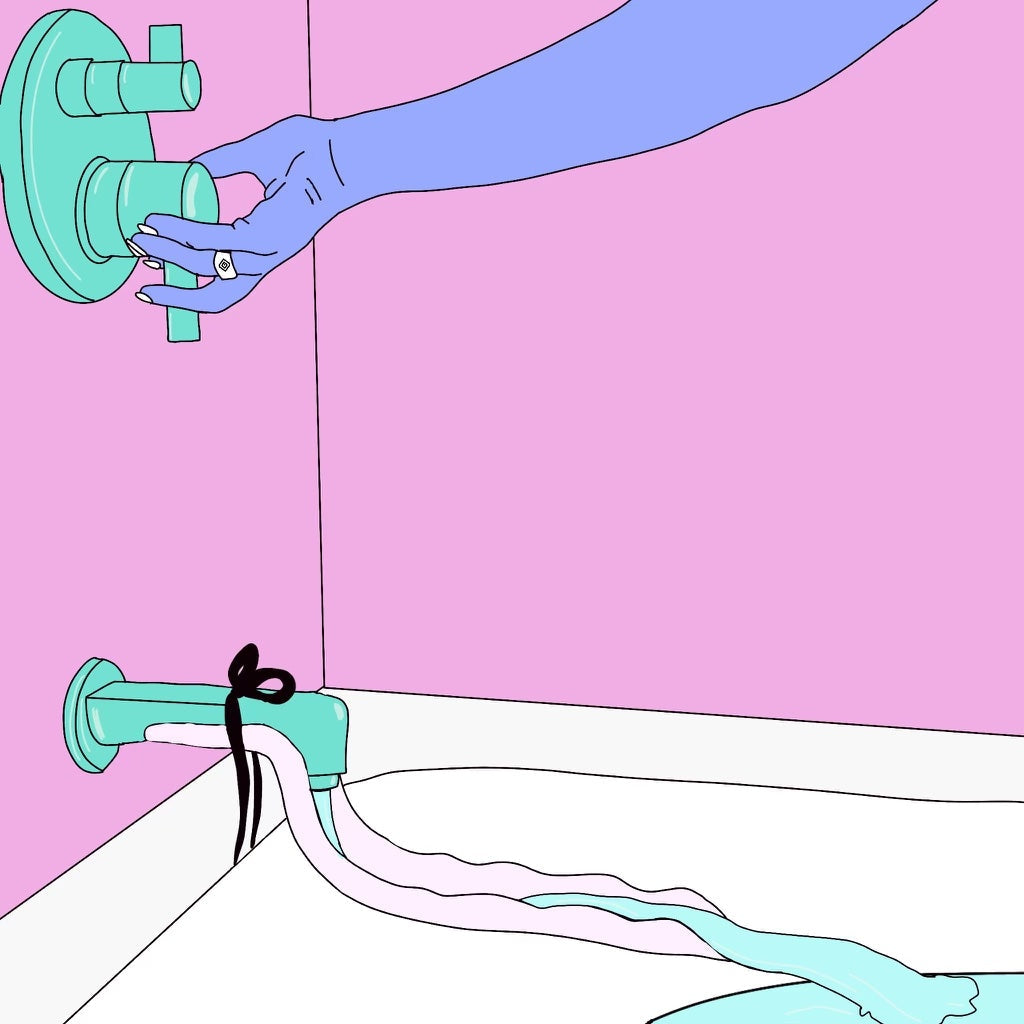
How To Use The WaterSlyde | Bathtub Masturbation Tips & Tricks
A step-by-step guide and tips and tricks for how to use the WaterSlyde aquatic stimulator, the patented bathtub faucet attachment that turns your bathtub into your favorite sex toy!
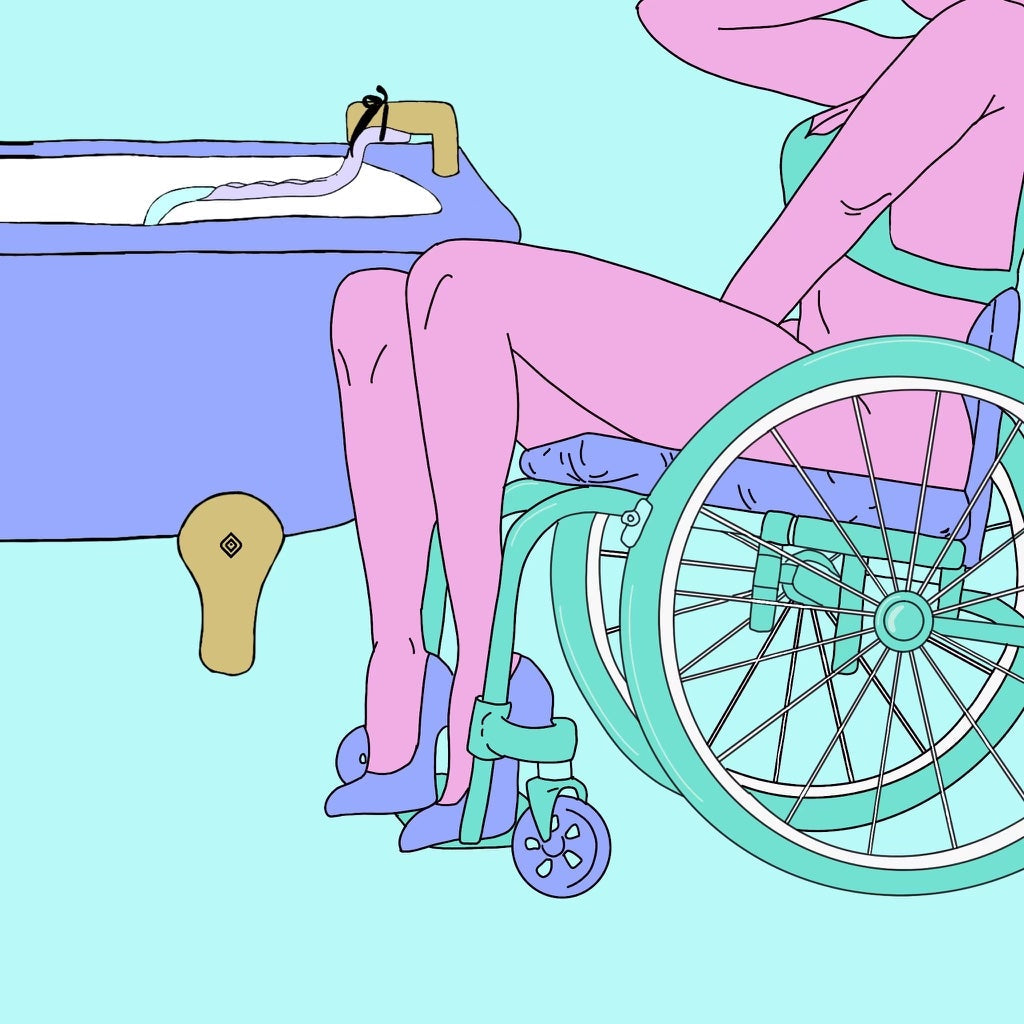
Meet The World's Most Disability-Friendly Sex Toy
Engaging in sexual activity is an essential part of every person's quality of life, not just the able-bodied. Typical vibrators and dildos require some level of physical dexterity and manual strength that not all of us possess or desire. Meet the WaterSlyde, the world's most disability-friendly sex toy.
How A Stay-At-Home Mom Overcame Fear And Invented A Game-Changing Sex Toy
Maureen Pollack, a wife and mother of 2 kids, was up against it when she decided to invent and patent The WaterSlyde, a water diverter that enables women to comfortably enjoy bathtub masturbation. With determination, she overcame her fears and created the world's most body-safe and eco-friendly pleasure product.
The Girls Who Get It: 17 Hysterical Comments From The WaterSlyde's Latest Viral TikTok
With over 25M views and 16K comments, the WaterSlyde's latest TikTok viral post confirms that bathtub masturbation is enjoyed by women everywhere.
How To Masturbate On Your Period Without Making A Mess
Here are a few tips and tricks for how to masturbate on your period without making a mess (i.e., leaving behind a full-blown crime scene!).